Content
Boost testosterone with personalized treatment plans
Primary vs. Secondary Hypogonadism Explained: How They Differ and What It Means for Your Health
Key Takeaways:
Male hypogonadism means your body isn’t making enough testosterone, the hormone that plays a role in sex drive, energy, and muscle strength.
Primary hypogonadism starts with problems in the testes, while secondary hypogonadism happens due to disrupted hormone signaling between the brain and testes.
Both types share symptoms, but primary hypogonadism usually impacts fertility, while secondary hypogonadism has a connection with conditions like type 2 diabetes and obesity.
Treatment depends on the cause and may include testosterone therapy or other medications.
Male hypogonadism is surprisingly common, affecting about 1 in 3 men over 45.
There are two main types: primary and secondary hypogonadism. One type starts in the testes, while the other has to do with a communication problem between the brain and testes.
Knowing which type you have helps your healthcare provider suggest the right treatment.
Read on to learn more about primary vs. secondary hypogonadism.
Content
What Is Hypogonadism?
Your testicles produce several different hormones — like estradiol, antimullerian hormone, progesterone, and testosterone.
Male hypogonadism is the medical term for low testosterone or low T. It means your testicles (your body’s hormone factories) aren’t working at full capacity, and not making enough testosterone.
Testosterone plays a major role in things like your sex drive, physical strength, mental sharpness, and even your mood. Without enough of it, everything from your well-being to your relationships can suffer.
If you have serum testosterone levels lower than 300 ng/dL, you might experience:
Low sex drive
Gynecomastia (breast development)
Decreased muscle mass
Less body hair
Low energy levels
Mood changes
Hot flushes
Difficulty concentrating
Reduced bone density
Low sperm count
What Is Primary Hypogonadism?
Primary hypogonadism happens when the testicles can’t make enough testosterone, even though hormones like follicle-stimulating hormone (FSH) and luteinizing hormone (LH) are high.
This is sometimes called primary testicular failure or hypergonadotropic hypogonadism.
Potential causes of primary hypogonadism include:
Genetic conditions (like Klinefelter syndrome)
Infections (like mumps)
Damage from radiation therapy, chemotherapy, or prostate cancer treatment
Medical conditions like hemochromatosis (iron overload)
Testicular injury
Undescended testicles
Aging
What Is Secondary Hypogonadism?
Secondary hypogonadism is when the brain — specifically the hypothalamus or pituitary gland — doesn’t send the proper signals to the testicles, leading to low testosterone.
With this type, FSH and LH are low or slightly below normal.
Potential causes of secondary hypogonadism include:
Genetic conditions (like Kallmann syndrome)
Pituitary tumors
High prolactin levels
Head injury
Stress
Health issues like type 2 diabetes, obesity, or sleep apnea
Steroid use
HIV
Here’s a glance at the key differences between primary and secondary hypogonadism:
Drug | Injection or pill | FDA-approved for |
|---|---|---|
Ozempic® | Weekly injection | Type 2 diabetes |
Wegovy® | Weekly injection | Weight loss |
Zepbound® | Weekly injection | Weight loss |
Saxenda® | Daily injection | Weight loss |
Metformin | Daily pill | Type 2 diabetes |
How They Impact the Body Differently
Both primary and secondary hypogonadism lower your androgen levels, causing similar symptoms like:
Low sex drive
Decreased muscle massReduced body hair
Mood changes
But they impact the body differently.
Primary hypogonadism often leads to fertility problems, low sperm count, smaller testicles, and sometimes enlarged breast tissue.
With secondary hypogonadism, there’s usually a connection to other health conditions like obesity, higher body fat, type 2 diabetes, and sleep apnea.
Low T shows up with both types of hypogonadism. Here’s how healthcare providers figure out which type you have:
Blood Tests
Your provider might order blood tests to check total testosterone, LH, FSH, sex hormone-binding globulin. These results tell your provider where the issue is stemming from: your testes or your brain. Your provider might also check your iron levels if they suspect an underlying issue like too much iron in your body.
Genetic Testing
If your provider suspects a genetic root cause, they might refer you to a specialist. A karyotype test can spot chromosome issues like Klinefelter syndrome.
Imaging
Sometimes, an MRI or CT scan is needed to see if your hypothalamus or pituitary gland looks abnormal.
Want to check your T levels without leaving the house? Hims offers an easy, convenient at-home testosterone test — so you can get answers, fast, and follow-up with a healthcare provider for next steps.
Treatment Approaches
Identifying whether you have primary or secondary hypogonadism is important because it can help guide your treatment. While you can manage both with testosterone replacement therapy, other treatment strategies are an option, too.
Treatment for Primary Hypogonadism
When the testes can’t make enough testosterone on their own, treatment usually focuses on replacing the missing hormone. Here’s what your provider might suggest:
Testosterone replacement therapy (TRT). Testosterone therapy comes in a variety of forms, including injections, gels, patches, pills, or testosterone pellets. Most men with primary hypogonadism need lifelong TRT.
Fertility treatments. Both primary hypogonadism and TRT can impact sperm production and increase your risk for infertility. Assisted reproductive technologies (ART) like in vitro fertilization (IVF) can help if you’re actively trying to have kids.
Erectile dysfunction medications. While ED medications like Viagra® (sildenafil) and Cialis® (tadalafil) won’t raise your testosterone levels, they may help improve erectile function due to low testosterone levels.
Treatment for Secondary Hypogonadism
Since the problem lies in the brain’s signaling (the hypothalamic-pituitary system), treatment for secondary hypogonadism may involve both hormone therapy and treatment for underlying causes:
Testosterone replacement therapy. Similar to primary hypogonadism, TRT can help relieve symptoms.
Selective estrogen receptor modulators (SERMs). Medications like clomiphene citrate or enclomiphene citrate may help your body make natural testosterone, without impacting fertility.
Human chorionic gonadotropin (hCG). Like SERMs, hCG is a fertility-safe treatment for low testosterone.
Aromatase inhibitors. Medications like anastrozole and letrozole reduce estrogen, which can help increase serum testosterone concentrations.
Managing pituitary problems. If a pituitary tumor is the cause of hypogonadism, surgery or administration of pituitary hormones may be needed.
Erectile dysfunction medications. As with primary hypogonadism, erectile dysfunction medications may help improve this symptom of low T. Hims offers access to a 2-in-1 medication containing enclomiphene and tadalafil to improve testosterone and erectile function simultaneously.
Treatment for both primary and secondary hypogonadism also includes follow-up blood tests to check testosterone. Your provider will also order prostate-specific antigen (PSA) screening if you’re on TRT. That’s because there’s a link between elevated PSA levels and an increased risk of benign prostatic hyperplasia (enlarged prostate).
While lifestyle changes can’t increase your T levels, healthy choices can support your body’s ability to make its own testosterone. Learn more about increasing your testosterone naturally.
Bottom Line
Both primary and secondary hypogonadism lead to low testosterone, but the underlying causes can be very different. Primary starts in the testes, while secondary involves the brain’s signaling system.
Knowing which type you have matters, since it shapes your treatment plan — whether that’s long-term testosterone replacement therapy or fertility-preserving medications like enclomiphene.
If you’re experiencing symptoms of low testosterone, talk with a healthcare provider. Hims can connect you with a licensed provider who can recommend testing and treatment options that fit your needs.
How do doctors tell primary from secondary hypogonadism?
Diagnosis usually starts with blood tests. In primary hypogonadism, luteinizing hormone and follicle-stimulating hormone are high, while in secondary hypogonadism, they’re low or normal. Additional tests may check prolactin, pituitary imaging, or genetic factors like Kallmann syndrome.
What genetic conditions are linked to hypogonadism?
Klinefelter syndrome (extra X chromosome) is a common genetic cause of primary hypogonadism. Kallmann syndrome, which affects gonadotropin-releasing hormone, is a genetic cause of secondary hypogonadism.
Can hypogonadism raise the risk of prostate cancer?
There’s no current evidence that low testosterone causes prostate cancer. But, men if you’re starting testosterone treatment, your provider might order PSA testing to track your prostate health.
What health conditions are linked with secondary hypogonadism?
There’s a link between secondary hypogonadism and health conditions like type 2 diabetes, obesity, and pituitary disorders. Chronic illness and certain treatments like radiation therapy can also affect hormone signaling.
Is secondary hypogonadism reversible?
Sometimes. If factors like obesity or sleep apnea are impacting your testosterone, treating the underlying issue may help restore testosterone production.
Can lifestyle changes improve testosterone levels?
Exercising regularly, following a balanced diet, losing weight, and lowering your stress can support testosterone production. But they can’t raise levels on their own.
What are the treatment options besides testosterone replacement therapy?
For some men, medications like clomiphene citrate, enclomiphene citrate, or hCG can help raise natural testosterone production while preserving fertility.
8 Sources
- Carnegie CH. (2004). Diagnosis of hypogonadism: Clinical assessments and laboratory tests. https://pmc.ncbi.nlm.nih.gov/articles/PMC1472884/
- Dandona P, et al. (2010). A practical guide to male hypogonadism in the primary care setting. https://www.ncbi.nlm.nih.gov/books/NBK532933/
- Hypogonadism in men. (2022). https://www.endocrine.org/patient-engagement/endocrine-library/hypogonadism
- Jarvis TH, et al. (2014). Testosterone and benign prostatic hyperplasia. https://pmc.ncbi.nlm.nih.gov/articles/PMC4650459/
- Kumar PE, et al. (2010). Male hypogonadism: Symptoms and treatment. https://pmc.ncbi.nlm.nih.gov/articles/PMC3255409/
- Madhusoodanan VI, et al. (2019). Human chorionic gonadotropin monotherapy for the treatment of hypogonadal symptoms in men with total testosterone > 300 ng/dL. https://pmc.ncbi.nlm.nih.gov/articles/PMC6844348/
- Sizar OM, et al. (2024). Male hypogonadism. https://www.ncbi.nlm.nih.gov/books/NBK532933/
- Tajar AB, et al. (2010). Characteristics of secondary, primary, and compensated hypogonadism in aging men: Evidence from the European Male Ageing Study. https://academic.oup.com/jcem/article-abstract/95/4/1810/2597149?redirectedFrom=fulltext
Editorial Standards
Hims & Hers has strict sourcing guidelines to ensure our content is accurate and current. We rely on peer-reviewed studies, academic research institutions, and medical associations. We strive to use primary sources and refrain from using tertiary references. See a mistake? Let us know at [email protected]!
This article is for informational purposes only and does not constitute medical advice. The information contained herein is not a substitute for and should never be relied upon for professional medical advice. Always talk to your doctor about the risks and benefits of any treatment. Learn more about our editorial standards here.
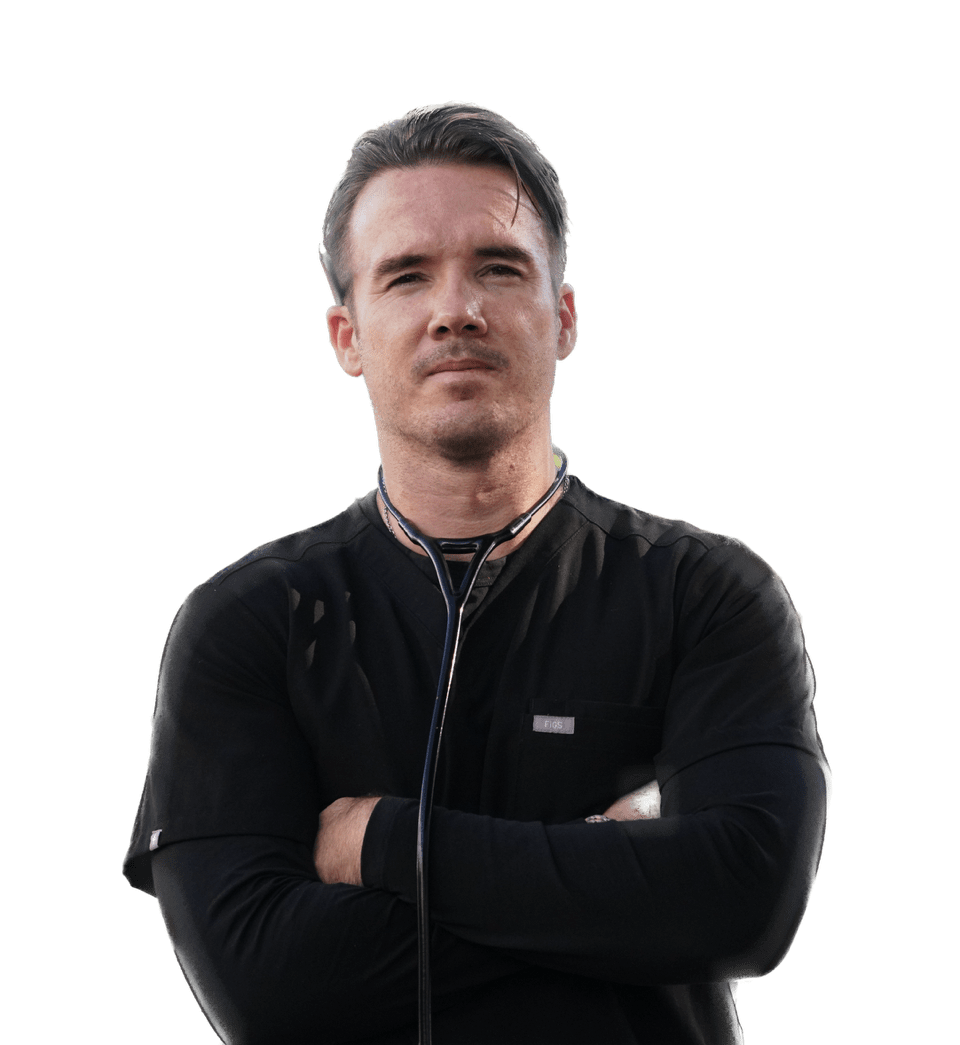
Darragh O’Carroll, MD
Basic Information
Full Name: Darragh O’Carroll MD
Professional Title(s): Board Certified Emergency Physician
Current Role at Hims & Hers: Medical Advisor
Credentials & Background
Education:
Bachelor of Science in Human Physiology - Boston University, 2007
Medical Doctorate - University of Hawaii John A. Burns School of Medicine, 2012
Training:
Internship & Residency - Los Angeles General + USC Emergency Medicine, 2016
Medical Licenses:
California, 2013
Hawaii, 2016
Board Certifications:
Experience & Expertise
Years of Experience: 14
Contributions to Hims & Hers
Medical Content Reviewed & Approved:
List pages or topics the expert has reviewed for accuracy
Media Mentions & Features:
Why I Practice Medicine
Health is never appreciated until it's gone. There’s nothing more satisfying than to save, change, or improve the health of someone in need.