Content
Labs by Hims is the key to a healthier you
How Hormones Affect Mood, Mental Health, Sleep, and Energy
Key Takeaways:
Hormones like testosterone, cortisol, melatonin, and more directly influence men’s mood, energy, and sleep quality.
Hormonal imbalances can cause depression, anxiety, irritability, fatigue, and sleep problems.
Men’s hormones follow a 24-hour cycle, with testosterone and cortisol peaking in the morning and declining at night.
Lifestyle factors, like diet, exercise, sleep, and stress, play a major role in maintaining healthy hormone balance.
Hormones are your body’s chemical messengers, and they’re working behind the scenes 24/7 to ensure all of your body’s systems are functioning appropriately. The influence of hormones extends to mental health, impacting sleep, mood, and energy levels.
When your hormones are in balance, they help you stay focused, motivated, and emotionally steady. But when levels dip too low, spike too high, or fall out of rhythm, the effects can show up as irritability, brain fog, fatigue, restless nights, or depression.
For men, testosterone, cortisol, melatonin, insulin, and thyroid hormones are especially influential for preserving mental health. Understanding how these hormones work can be the first step in protecting your overall well-being.
Content
Hormones are chemical messengers that travel through your bloodstream, carrying instructions from one part of the body to another. They help regulate nearly every biological system, from metabolism and growth to reproduction and mood.
The link between hormones and mental health is strong: Hormones directly influence how the brain functions and how you feel from day to day.
Stable hormone levels support steady energy, restorative sleep, and a balanced mood. But even small disruptions — like too much cortisol from chronic stress or declining testosterone with age — can tip the balance and lead to irritability, poor focus, fatigue, or symptoms of anxiety and depression.
In other words, hormone health is mental health. Understanding that connection makes it easier to recognize when something feels “off.”
Several hormones have a direct influence on mental health, sleep quality, and energy levels. Here’s how those key players work:
Testosterone
As the primary male sex hormone, testosterone supports mood stability, confidence, motivation, and cognitive sharpness. Low levels may connect to irritability, depression, reduced focus, and fatigue. Testosterone also helps to regulate sleep quality, with deficiencies linked to insomnia or restless sleep.
Cortisol
Known as the body’s stress hormone, cortisol helps to regulate energy, alertness, and the sleep-wake cycle. Short-term spikes help you handle challenges, but when levels stay high due to chronic stress or poor sleep, cortisol can also trigger anxiety, mood swings, and daytime exhaustion.
Melatonin
This hormone helps to regulate the body’s circadian rhythm — the natural 24-hour cycle that controls when you feel sleepy or alert. Declining melatonin with age or disrupted production (perhaps as a result of late-night screen time) can make falling or staying asleep more difficult. These scenarios can directly affect mood and energy.
Thyroid Hormones
Produced by the thyroid gland, this group of hormones regulates metabolism and energy production. Low levels of thyroid hormone (hypothyroidism) can lead to sluggishness, brain fog, and depression, while high levels (hyperthyroidism) may cause restlessness, irritability, and sleep problems.
Insulin
Best known for regulating blood sugar, insulin also impacts energy levels and brain health. When insulin doesn’t work properly (known as insulin resistance), energy crashes, mood swings, and fatigue often follow.
Serotonin
Serotonin functions in the body as both a neurotransmitter and a hormone. It interacts with the hormones estrogen, testosterone, and cortisol. Serotonin is also a key player in mood regulation, and imbalances can contribute to symptoms of depression, anxiety, or irritability.
When hormones fall out of balance, the effects often show up in three main areas: mood, sleep, and energy. Even subtle shifts can create a noticeable impact on day-to-day mental health.
Hormones and Mood
Hormonal imbalances are strongly tied to changes in mood and sometimes mood disorders. Low testosterone can cause irritability, apathy, or symptoms of depression, while chronically high cortisol may have associations with anxiety and mood swings. Thyroid disorders can mimic mental health issues, leading to either slowed thinking and sadness or nervousness and agitation.
Hormones and Sleep
Sleep quality is a common victim of various hormonal changes. Insufficient melatonin makes falling or staying asleep more difficult. Elevated cortisol at night can keep the brain in “alert” mode, leading to restless nights. And low testosterone has associations with poorer sleep quality and reduced restorative deep sleep.
Hormones and Energy
Hormones act like fuel regulators for the body. When thyroid levels are low, fatigue and sluggishness may set in. Insulin resistance can cause blood sugar crashes that drain energy and affect focus. Low testosterone contributes to overall exhaustion, while poor sleep from hormonal issues only makes fatigue worse.
Men’s 24-Hour Hormone Cycle
Men’s hormones don’t stay static throughout the day. Rather, they follow natural fluctuations that influence energy, focus, and mood. Two of the most important are testosterone and cortisol, both of which follow a roughly 24-hour cycle.
Testosterone peaks in the early morning hours, supporting alertness, motivation, and sexual health. Levels gradually decline as the day goes on, often hitting their lowest point in the evening. This is one reason men may feel sharper and more energized earlier in the day.
Cortisol, the stress hormone, also follows a daily pattern. It rises sharply in the morning to help you wake up and feel alert, then steadily declines throughout the day, reaching its lowest levels at night to allow for restful sleep.
Together, these daily rhythms keep your body on track. But when they’re thrown off (by aging, stress, poor sleep, or medical conditions), the result can be fatigue, brain fog, irritability, or low motivation.
Your daily habits play a big role in how well your hormones function. While some shifts are inevitable with age, lifestyle choices can either support or disrupt hormonal balance.
Food. A balanced diet rich in whole foods, fiber, and healthy fats helps support normal levels of insulin, thyroid hormones, and testosterone. Too much ultra-processed food (items high in added sugar, sodium, and saturated fat, but low in nutrition) can encourage insulin resistance and energy crashes.
Exercise. Regular physical activity (not too little, but not too much) boosts testosterone, improves insulin sensitivity, and helps manage cortisol. Both strength training and aerobic exercise are important to include in your routine.
Sleep. Quality sleep is essential for restoring testosterone, melatonin, and cortisol rhythms. Skimping on rest disrupts these cycles, which can lead to fatigue, mood issues, and poor concentration.
Stress. Chronic stress keeps cortisol elevated, which can interfere with sleep, testosterone production, and overall mental health. Practices like meditation, deep breathing, or regular downtime help to regulate stress hormones.
Alcohol. Drinking can disrupt testosterone production, impair thyroid function, and interfere with sleep-regulating hormones like melatonin.
Testing Hormones for Mental Health
If you’re dealing with ongoing fatigue, mood swings, low energy, or sleep issues, hormone testing can help identify whether imbalances are part of the root problem.
Blood tests are the most common way to measure hormone levels, and your healthcare provider can recommend which labs make sense to order based on your symptoms.
Common lab tests include:
Testosterone panel. Measures total and free testosterone levels to check for deficiencies.
Thyroid panel (TSH, free T3, free T4). Evaluates thyroid function, which plays a major role in metabolism, mood, and energy.
Cortisol levels. May be tested with a blood draw or a saliva test to assess stress response and daily rhythm.
Insulin and HbA1c. Provide insight into blood sugar regulation, which affects energy and mood stability.
Getting the right labs can clarify whether your symptoms stem from a hormonal imbalance or another health condition. Results — interpreted in context by a healthcare provider — can help guide your next steps for treatment.
If testing shows an imbalance, the good news is that there are many ways to bring hormone levels back into a healthy range. Treatment often combines lifestyle adjustments with targeted medical support, when needed.
Lifestyle Changes
Prioritizing quality sleep, exercising regularly, managing stress, and eating a nutrient-rich diet are the foundations for healthy hormone production. These changes alone can often improve mild imbalances.
Medical Treatments
For more significant issues, healthcare providers may recommend options like testosterone replacement therapy, thyroid medications, or insulin-sensitizing drugs.
Using supplements such as melatonin on a short-term basis may help to regulate sleep cycles, though research on its effectiveness is mixed.
Monitoring and Follow-Up
Restoring balance usually requires lab checks and adjustments over time. Partnering with a healthcare provider ensures that treatment supports both physical and mental health safely.
When addressed early, restoring hormone balance can improve not only mood, sleep, and energy, but also long-term health and quality of life, which is your ultimate goal.
Hormones are deeply tied to men’s mental health, influencing mood, energy, and sleep on a daily basis. Even slight imbalances in testosterone, cortisol, thyroid hormones, or melatonin can ripple through the body and affect well-being.
Paying attention to symptoms, getting tested when needed, and making lifestyle changes, or seeking medical support, can help restore balance. If your mood, sleep, or energy feels off, talk with a healthcare provider about whether hormones could be part of the issue.
FAQs
We’ve compiled some questions guys commonly ask about the link between their hormones and mental well-being.
Can hormones affect mental health?
Yes. Hormones like testosterone, cortisol, thyroid hormones, and melatonin all influence mood, sleep, and energy. Imbalances in these hormones can contribute to symptoms of depression, anxiety, irritability, and fatigue.
Can hormones affect sleep?
Absolutely. Melatonin helps to regulate your body’s sleep-wake cycle, while cortisol and testosterone also play roles in sleep quality. Low or disrupted levels of these hormones can lead to insomnia, restless sleep, or difficulty staying asleep.
Which hormones affect mood the most?
Testosterone, cortisol, and thyroid hormones are especially linked to mood regulation. When these hormones are out of balance, men may be more likely to experience depression, anxiety, irritability, or brain fog.
How do I know if my hormones are out of balance?
Common signs of hormone imbalance include low energy, sleep problems, mood swings, changes in weight, or reduced concentration. If you’re experiencing ongoing symptoms, your doctor can order blood tests to check your hormone levels.
What is the men’s 24-hour hormone cycle?
Men’s testosterone and cortisol levels naturally peak in the morning and decline throughout the day. This rhythm helps regulate energy, focus, and sleep, but stress, aging, or poor lifestyle habits can disrupt it.
How can I improve my hormone health naturally?
Prioritizing sleep, exercising regularly, eating a balanced diet, and managing stress all support hormone balance. Avoiding excess alcohol can also help maintain healthy levels.
When should I get my hormones tested?
If you’re experiencing persistent fatigue, depression, anxiety, low sex drive, or poor sleep, talk to your healthcare provider about hormone testing. Blood work can identify certain imbalances and guide treatment.
34 Sources
- Begemann K, et al. (2025). Endocrine regulation of circadian rhythms. https://doi.org/10.1038/s44323-025-00024-6
- Bonmati-Carrion MA, et al. (2014). Protecting the melatonin rhythm through circadian healthy light exposure. https://pubmed.ncbi.nlm.nih.gov/25526564/
- Chen Z, et al. (2023). Ultra-Processed Food Consumption and Risk of Type 2 Diabetes: Three Large Prospective U.S. Cohort Studies. https://diabetesjournals.org/care/article/46/7/1335/148548/Ultra-Processed-Food-Consumption-and-Risk-of-Type
- Costello RB, et al. (2014). The effectiveness of melatonin for promoting healthy sleep: a rapid evidence assessment of the literature. https://pmc.ncbi.nlm.nih.gov/articles/PMC4273450/
- Crawford ED, et al. (2015). Measurement of testosterone: how important is a morning blood draw?. https://pubmed.ncbi.nlm.nih.gov/26360789/
- de Almeida Ferreira M, et al. (2022). Long-term testosterone replacement therapy reduces fatigue in men with hypogonadism. https://pmc.ncbi.nlm.nih.gov/articles/PMC8823386/
- Depino A, et al. (n.d.). Hormone and mood disorders. https://www.nature.com/collections/dciefdeije
- Dziurkowska E, et al. (2021). Cortisol as a Biomarker of Mental Disorder Severity. https://pmc.ncbi.nlm.nih.gov/articles/PMC8584322/
- Freeman AM, et al. (2023). Insulin Resistance. https://www.ncbi.nlm.nih.gov/sites/books/NBK507839/
- Green ME, et al. (2021). Thyroid Dysfunction and Sleep Disorders. https://pubmed.ncbi.nlm.nih.gov/34504473/
- Hackney AC, et al. (2015). Exercise and the Regulation of Endocrine Hormones.Prog Mol Biol Transl Sci. 2015;135:293-311. doi:10.1016/bs.pmbts.2015.07.001 https://pubmed.ncbi.nlm.nih.gov/26477919/
- Jansen HI, et al. (2023). Hypothyroidism: The difficulty in attributing symptoms to their underlying cause. https://pmc.ncbi.nlm.nih.gov/articles/PMC9939761/
- Jiao Y, et al. (2025). Sleep disorders impact hormonal regulation: unravelling the relationship among sleep disorders, hormones and metabolic diseases. https://doi.org/10.1186/s13098-025-01871-w
- Johnson J, et al. (2013). The Effect of Testosterone Levels on Mood in Men: A Review. https://doi.org/10.1016/j.psym.2013.06.018
- Kaltsas G, et al. (2010). Fatigue, endocrinopathies, and metabolic disorders. https://pubmed.ncbi.nlm.nih.gov/20656620/
- Kim TW, et al. (2015). The impact of sleep and circadian disturbance on hormones and metabolism. https://pubmed.ncbi.nlm.nih.gov/25861266/
- Koncz A, et al. (2021). Meditation interventions efficiently reduce cortisol levels of at-risk samples: a meta-analysis. https://pubmed.ncbi.nlm.nih.gov/32635830/
- Kumar R, et al. (2023). The Association Between Thyroid Stimulating Hormone and Depression. https://www.mayoclinicproceedings.org/article/S0025-6196%2823%2900012-5/abstract
- Kurhaluk N. (2021). Alcohol and melatonin. https://pubmed.ncbi.nlm.nih.gov/33761823/
- Kuś A, et al. (2021). Thyroid Function and Mood Disorders: A Mendelian Randomization Study. https://pubmed.ncbi.nlm.nih.gov/33899528/
- Lange J, et al. (2025). HPA system in anxiety disorder patients treated with cognitive behavioural therapy: A review. https://doi.org/10.1016/j.bionps.2024.100116
- Määttänen I, et al. (2021). Testosterone and specific symptoms of depression: Evidence from NHANES 2011-2016. https://pmc.ncbi.nlm.nih.gov/articles/PMC9216439/
- McEwen BS. (2008). Central effects of stress hormones in health and disease: Understanding the protective and damaging effects of stress and stress mediators. https://pmc.ncbi.nlm.nih.gov/articles/PMC2474765/
- Patel P, et al. (2019). Impaired sleep is associated with low testosterone in US adult males: results from the National Health and Nutrition Examination Survey. https://pubmed.ncbi.nlm.nih.gov/30225799/
- Perfalk E, et al. (2017). Testosterone levels in healthy men correlate negatively with serotonin 4 receptor binding. https://pubmed.ncbi.nlm.nih.gov/28426945/
- Rivas AM, et al. (2014). Diagnosing and managing low serum testosterone. https://pmc.ncbi.nlm.nih.gov/articles/PMC4255853/
- Salvador J, et al. (2021). Endocrine Disorders and Psychiatric Manifestations. https://doi.org/10.1007/978-3-319-68729-2_12
- Smith SJ, et al. (2023). The effects of alcohol on testosterone synthesis in men: a review. https://pubmed.ncbi.nlm.nih.gov/36880700/
- Stalder T, et al. (2025). The Cortisol Awakening Response: Regulation and Functional Significance. https://pubmed.ncbi.nlm.nih.gov/39177247/
- Thau L, et al. (2023). Physiology, Cortisol.https://www.ncbi.nlm.nih.gov/books/NBK538239/
- Young AH. (2004). Cortisol in mood disorders. https://pubmed.ncbi.nlm.nih.gov/16019585/
- Zhang Y, et al. (2023). Ultra-processed foods and health: a comprehensive review. https://pubmed.ncbi.nlm.nih.gov/35658669/
- Zisapel N. (2018). New perspectives on the role of melatonin in human sleep, circadian rhythms and their regulation. https://pmc.ncbi.nlm.nih.gov/articles/PMC6057895/
- Zitzmann M. (2020). Testosterone, mood, behaviour and quality of life. https://pubmed.ncbi.nlm.nih.gov/32657051/
Editorial Standards
Hims & Hers has strict sourcing guidelines to ensure our content is accurate and current. We rely on peer-reviewed studies, academic research institutions, and medical associations. We strive to use primary sources and refrain from using tertiary references. See a mistake? Let us know at [email protected]!
This article is for informational purposes only and does not constitute medical advice. The information contained herein is not a substitute for and should never be relied upon for professional medical advice. Always talk to your doctor about the risks and benefits of any treatment. Learn more about our editorial standards here.
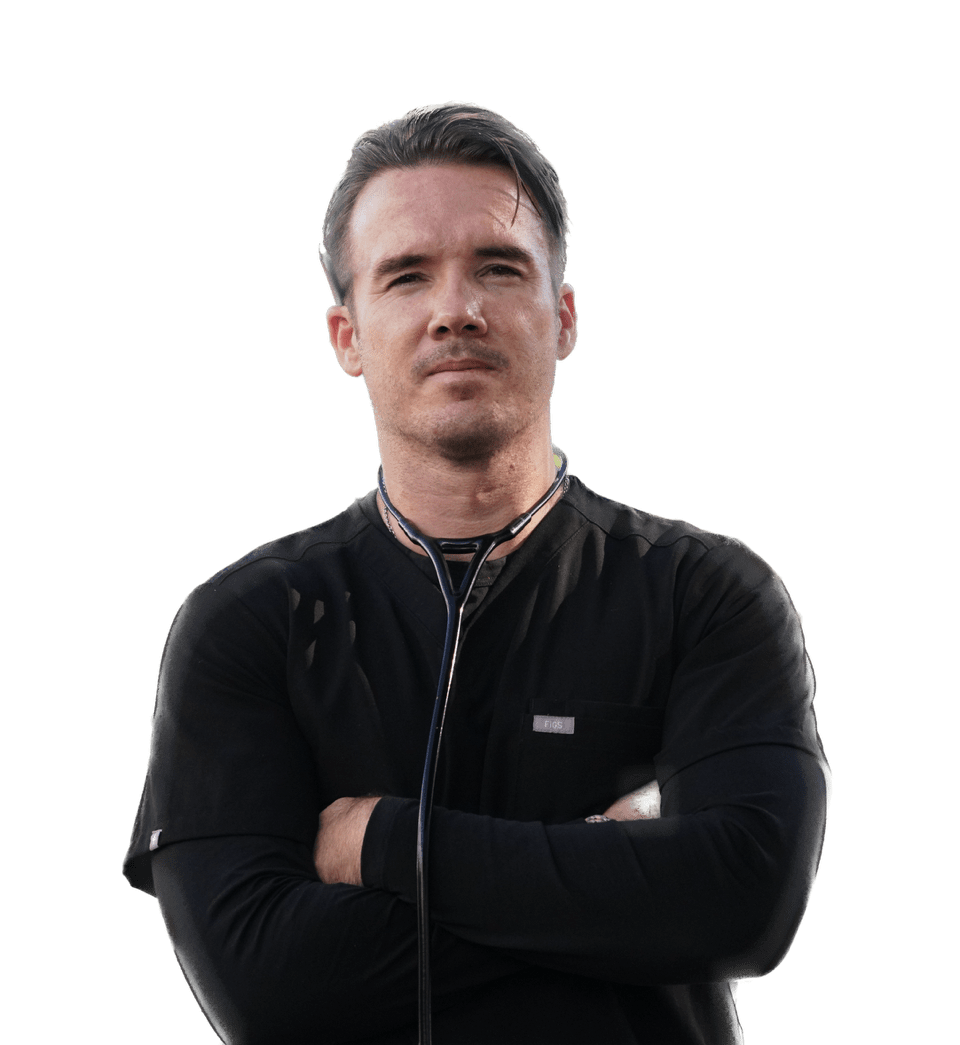
Darragh O’Carroll, MD
Basic Information
Full Name: Darragh O’Carroll MD
Professional Title(s): Board Certified Emergency Physician
Current Role at Hims & Hers: Medical Advisor
Credentials & Background
Education:
Bachelor of Science in Human Physiology - Boston University, 2007
Medical Doctorate - University of Hawaii John A. Burns School of Medicine, 2012
Training:
Internship & Residency - Los Angeles General + USC Emergency Medicine, 2016
Medical Licenses:
California, 2013
Hawaii, 2016
Board Certifications:
Experience & Expertise
Years of Experience: 14
Contributions to Hims & Hers
Medical Content Reviewed & Approved:
List pages or topics the expert has reviewed for accuracy
Media Mentions & Features:
Why I Practice Medicine
Health is never appreciated until it's gone. There’s nothing more satisfying than to save, change, or improve the health of someone in need.